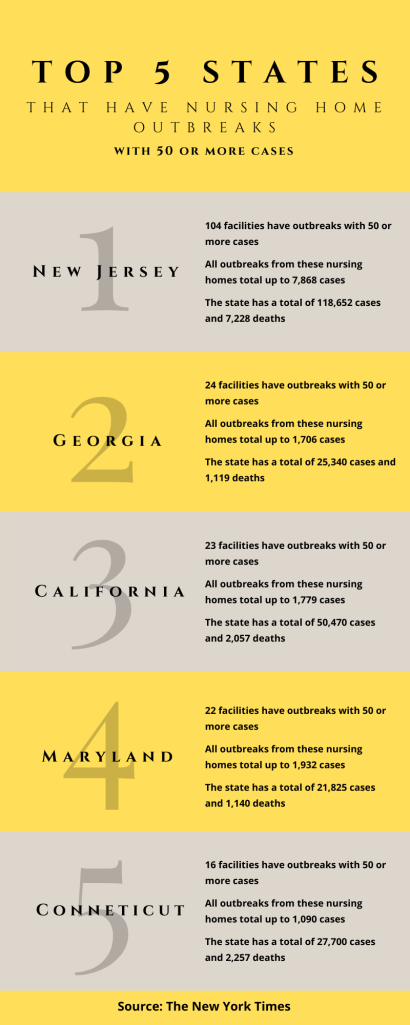
WALKERSVILLE, Md. — Nursing homes and other long-term care facilities continue to be major hotspots for coronavirus outbreaks in the US. The New York Times has found that more than 5,700 long-term care facilities have been affected with coronavirus cases. In Maryland, nursing home outbreaks have resulted in 1,547 cases and 8 deaths among staff and 3,372 cases and 546 deaths among residents, according to data from the state government. The same data shows that in Frederick County, Maryland, where there are there are around 20 long-term care facilities, there have been 351 cases and 48 deaths among nursing home staff and residents.
According to the Centers for Disease Control and Prevention, older adults and those who have underlying health conditions are at higher risk for developing serious complications from the coronavirus. Of the deaths reported in the US, eight out of ten have been in adults aged 65 or older. The CDC notes that nursing home populations are at the highest risk of being infected by the virus, since they have high populations of older adults.
This news has caused a lot of concern among nursing home staff members, who have had many new policies and changes, some without their knowledge, or even consideration. New rules and regulations have continued to be applied to the essential workers, especially with the Maryland governor’s executive order regarding nursing homes and the state’s secretary of health’s own directive order, These orders have given nursing homes regulations that they must abide by, and failure to do so is a misdemeanor.
Some nursing home staff have shared how new policies from their individual facilities are affecting them amid the pandemic. All sources’ names have been changed and have asked that their places of work remain unnamed for confidentiality purposes.
Susan worked at both a hospital and a nursing home before the pandemic. Once the coronavirus started to become more serious, she was told she could not work at the nursing home anymore. She explained that there was a main and very important difference she’s seen between working at the hospital versus working at the nursing home, both before and during the pandemic: shared governance. Shared governance is a type of nursing practice that allows nurses to be a part of decision-making processes, according to an article by Dr. Mary K. Anthony. Susan* explained that, while the hospital modeled shared-governance, nursing homes lacked it.
At the hospital where Susan works, nurses and staff can bring up issues and suggestions and are allowed to help govern what policies get implemented for the patients. She said that the hospital has even formed a command center for COVID-19 where these suggestions and concerns can be posted and nurses can speak to experts, as well as receive training and other materials to help combat the outbreak.
However, the same cannot be said for nursing homes. In nursing homes, what is beneficial for the residents is not always getting relayed to the people who make the “big decisions.” Nurses are not a part of the decision-making process and often cannot bring issues and suggestions to administration. Susan believes that every nursing home should not only have a form of shared governance, but should also have a similar program like her hospital’s COVID-19 command center. “It is the best thing for our community,” she said. “It can really help everyone, from the residents to the staff to the facility as a whole and can help combat what we are going through right now.”
Lucy’s* nursing home has a few deaths from the virus and multiple cases among both residents and staff, according to data from the government. She is very upset with how her nursing home administration has chosen to handle the pandemic. According to her, the staff are kept in the dark. “We don’t know which of us or the residents are infected,” she says. “It’s really scary and it can cause more outbreaks if we don’t know who we should be careful around.”
Lucy explains that another main issue that has been plaguing the workers is who gives the residents their medicine and baths, which has changed due to a recent change in management due to the pandemic.
Lucy’s facility has four floors, and each floor has around 30 rooms, she says. “Under our previous manager, we would have at least one person working a floor, giving the residents on that floor their medications during their shifts,” she said. “Now, they have one nurse working two floors.” She says that this has caused many issues, stemming with the nurses now being required to rush around from floor to floor to make sure all the residents get their medications in time.
The nurses are not even allowed to use the elevators, but that is not Lucy’s main concern. “Before this new policy, we had time to be able to talk to the residents and make them feel like this is a home to them,” she said. “The residents don’t hear from their family all the time and some of them don’t even have family that come to visit. We, the nurses and staff, are their family.”
Lucy says that, now, the nurses don’t have time to interact with the residents. If the residents want to talk, they can’t, because they have to run to get another resident tehir medicine. “It really breaks my heart,” she says. “All of this is happening, and we can’t even complain — or offer suggestions. How will anything change?”
Riley* said that in his nursing home, staff are also not really a part of the decision making and are kept in the dark about a lot of things. “We’re told that there are meetings to discuss policies and new changes, but we don’t even know about the meetings or any new policies until we get to work at the time of our individual shifts,” he said. “There are some policies that I feel don’t address actual concerns that we as the nurses have brought up.” He explained that this doesn’t surprise him however, since the administrators making decisions are not actually working with the residents and in the same settings the nurses are.
Riley said that it feels like the nursing home administrators only care about profit now. He explained that he has been talked to about making sure to clock out a specific time, even if he can’t leave yet because he is still working. “They don’t even want to pay us our overtime anymore, much less pay us if anything actually happens to us,” he said. He explained that workers have both paid time off and catastrophe time off. Catastrophe time off is used for an emergency — when a worker is sick or hospitalized, when they can’t come to work for something uncontrollable. Paid time off is typically used when a worker knows they are going to miss work, such as for vacation. “If we get sick from the virus, my work will not pay me using the catastrophe time off hours,” he said. “It will be with my paid time off and, once that is finished, I’m out of means to get paid and take care of my family.”
Mary* works as a dietary nutritionist at her nursing home. She says that her nursing home underwent similar circumstances as the another’s; the residents must stay in rooms, no visitations, and a complete lockdown.
“In the first few weeks, we were allowed to bring the residents their food,” she said. “But now the nurses take them their food. We don’t even get to leave the dining hall; we just prepare the food and make sure it’s ready for the nurses.”
Although Mary knows some protocols are for the safety of the residents, she says that she wishes the administration would ask for at least an opinion from the workers. “They don’t let us tell them anything really, and they hardly tell us anything,” she said. “I feel bad for the residents, being locked in their rooms with no information on what’s even going on. We can’t even help them aside from our immediate jobs.”
Mary agrees that the administration should not be the only ones making all the decisions because they do not work directly with the residents; the nurses and rest of immediate staff do. She said that, although new policies made by her administration have not affected her directly, she has seen them affect others. She explained how one of her coworkers wanted to take a few days off to be with her mother who has cancer. “Our immediate manager said that she could,” she said. “But our manager’s manager said no, then pretty much told her she was fired if she did take those days off.”
With all of these new policies and the concerns from the staff, one can only wonder what is going to become of the US’s nursing homes, much less those in Maryland.
Riley said that one of his bosses told him that about 90 percent of Frederick County, Maryland’s nursing homes have at least one case of the coronavirus. He said that most nursing homes have adopted policies that could lead you to unemployment: if a worker has worked in a place with a case, they cannot go to their other place of work; and if a family member gets the virus or works in a place that has many cases, they may be asked to stay home. “It’s scary,” he said. “We’re not told anything, and I don’t know what the next day could bring. I don’t know if my wife or I may get a call that tells us not to come to work anymore.”
This is informative and very thoroughly reported! I didn’t see any major changes, except you might include a sentence or paragraph about the particular risks that COVID poses to senior citizens and those with underlying health conditions, and emphasize the situation (90 percent of homes with cases) in Frederick County higher in your article, if that’s where all your sources work. (I’m not sure about the graphic at the very top — beside looking overly cheerful for the topic, it suggests that nurses’ needs are being balanced with admins’, which doesn’t seem to be the case in your article.)
LikeLike
p.s. Also your headline could be more specific — “Covid outbreak raises concerns in nursing-home governance,” or something along those lines. 🙂
LikeLike
Just saw this article that may be interesting to you! https://www.washingtonpost.com/local/maryland-coronavirus-outbreak-in-nursing-homes/2020/05/06/178e4ff4-8d42-11ea-a0bc-4e9ad4866d21_story.html
LikeLike